Detecting Skin Cancer: The Importance of Being Naked
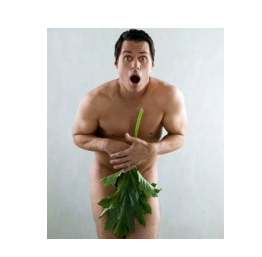
It’s true! Scientists have proven that being nude can save your life! Every adult should completely disrobe for a complete skin cancer evaluation. Contrary to popular lay opinion, skin cancers do not necessarily develop only in areas of the body exposed to the sun. In fact, there are skin cancers that tend to occur mainly on the skin, not exposed to the sun, making the importance of having a thorough dermatological examination paramount. This is especially true if you have a mutation for the BRAF or NRAS genes which predispose you to having melanoma. A complete skin examination should include the scalp, inside your ears, nails, inside your mouth, under the breasts, the genital areas, between your toes, as well as the obvious areas such as face, arms, legs, chest, and back.
Just this past year, I diagnosed 4 cases of squamous cell carcinoma on the penis. All 4 men vigorously denied having noticed any skin abnormalities in the genital region and initially refused to remove their underpants for skin examination. Three of the patients did not recognize the skin cancers on their penis despite my pointing it out and the fourth person’s lesion was so large that it was difficult to believe he didn’t see it. He said he “forgot it was there” after I showed it to him.
Fortunately, all these penile cancers were diagnosed at an early stage and were cured with simple surgical removal. However, squamous cell carcinoma of the penis can have high morbidity and result in penectomy or worse if diagnosed in an advanced stage.
I employ epiluminesence microscopy to check for abnormal pigment patterns that may be present in moles and unusual growths. This technique provides detailed magnification beyond what you can see with the naked eye; making the detection of skin cancers more accurate.
Types of Skin Cancers
- Melanoma
- Basal cell carcinoma
- Squamous cell carcinoma
- Atypical fibroxanthoma
- Merkel cell carcinoma
- Kaposi sarcoma
- Sebaceous carcinoma
- Cutaneous lymphomas
- Leukemias
- Paget’s Disease
- Liposarcoma
- Dermatofibromosarcoma Protuberans
- Leiomyosarcoma
- Angiosarcoma
- Microcystic adnexal carcinoma
- Metastatic carcinoma to the skin
WHAT YOU SHOULD DO TO PREPARE FOR YOUR SKIN EXAM:
Make a list ahead of time of any changes on your skin you have noticed, such as: (1) moles changing in shape, size, color, itching, bleeding, or causing pain, (2) new moles or growths and (3) any skin sores or pimple
type lesions that have not healed or gone away for several months.
Bring in all of your medications and skin care products that you are using on your skin.
If this is not practical to do, then make a written list of what you are using, where you are applying it, how often, and the reason you are using it. I see so many people who have seen another physician and then are seeing me for a second opinion and are unable to tell me what was prescribed. Describing the medication as a “white cream” is not helpful. It is impossible to intelligently guess what this might be since most of the topical medications are white. If possible, do not wear make-up or if you do, be prepared to wash it off for the office visit. Bring your make-up with you so you can reapply it after the visit.
Precancers and early skin cancers can be subtle and can be hidden by make-up.
Remove nail polish before your exam.
Melanomas can occur in the nail beds and will not be diagnosed if the nails are painted. Melanomas involving the nails are at high risk for distant metastases. Clear nail polish is fine to wear for the exam. Do not wear lots of jewelry. You will be asked to remove it for the exam. And finally, remember what your mother told you, wear your nice underwear to see the doctor!
Guidelines for how often to have a Skin Exam
You should have an annual skin examination if you have had:
- No Prior history of skin cancer
- Family history of melanoma
- History of moderate sun exposure-lots of fun in the sun in your younger years
- History of 3 or more sunburns at anytime
- 50 or more moles
You should be examined every 6 months if you have:
- Ongoing treatment for precancers
- Moderate sun damage
- History of non-melanoma skin cancer in past years
- Atypical or Dysplastic Moles
- History of 3 or more family members with melanoma indicates high risk genetic risk for melanoma
You should be examined every 4-6 months if you have had:
- Personal history of melanoma
- Any diagnosed skin cancer within the past 1-2 years
“BUT I HAVE THE GOOD KIND OF CANCER, RIGHT?”
As most of us know melanoma is a potentially fatal type skin cancer. What you may not realize is that having any skin cancer, it doesn’t have to necessarily be a melanoma, puts you at increased risk for developing melanoma in the future. Also, we now know that people who have been diagnosed with a nonmelanoma skin cancer are at high risk for other cancers such as lung, colorectal, breast and prostate cancer. So it is important to have a complete physical exam with your internist to be monitored for potential signs of cancer in these organs.
New skin cancers do not necessarily develop in the same areas as where you have had prior skin cancers. It is important to have a full body skin check and not limit the exam to the surgical site where a previous skin cancer was removed. Having had one skin cancer puts you at risk for developing another skin cancer but it does not in any way predict the site where the next cancer may occur. Your risk of developing melanoma is increased approximately 8 fold if you have had a non-melanoma skin cancer such as a basal cell carcinoma or a squamous cell carcinoma. Current data suggests that nonmelanoma skin cancer may be a marker of a high cancer risk phenotype regardless of sun exposure history.
Risk Factors for Melanoma
- Having 50 or more moles present. The moles do not have to be atypical in appearance.
- Family history of melanoma- genetics
- Personal history of melanoma
- Any history of a non-melanoma type skin cancer such as a basal cell carcinoma or squamous cell carcinoma
- Ultraviolet radiation from sun exposure-strong correlation for developing a type of melanoma known as lentigo maligna melanoma
- Atypical mole syndrome
- Arsenic or mercury exposure
- Light colored skin, hair, and eyes
- Occupational: Construction workers, gardeners, and lifeguards