Make Love Not Warts
Genital warts are the most common sexually transmitted disease. The lifetime risk for infection in sexually active adults may be as high as 80%. More than 40 types of human papillomavirus (HPV) cause genital warts. There are 2 classes of HPV: low risk and high risk of malignant potential. HPV types 16,18, 31, 33,35,39,45,51,52,56,58,59,68 are associated with high risk of malignant transformation to squamous cell carcinoma. HPV enters the nucleus of skin cells and integrates its DNA into the normal cell's DNA. The virus replicates inside the cell undetected by the host's immune system. Viral proteins E6 and E7 inactivate p53, the host cell's tumor suppressor gene allowing it to freely replicate. Risk factors for persistent HPV infection include increasing age, infection with multiple types of HPV, and infection with high risk types. Infection with one HPV type increases one's risk of infection from other HPV types. High risk HPV causes anal, vulvar, vaginal, penile, cervical, and oropharyngeal (oral) cancers.
A large proportion of HPV infection is latent or not visibly apparent to the naked eye. Condoms provide some rotection against acquiring HPV. In males, the risk of genital HPV infection is associated with not being circumcised, having had more than 6 sexual partners, having sex with professional sexual workers, and having sex before age 17.

Genital warts resemble little growths of cauliflower or broccoli on the surface of the skin. They may be skin colored, pink, brown, tan, grey, or white. Size can vary from the size of a pin head to several inches in diameter.HPV cannot
be cultured. Most of the time genital warts will go away without treatment. However, persistence of genital warts can signal an infection with a high risk HPV and medical attention is recommended.
There are a number of treatments available. Recently, the FDA approved a new topical medication that contains sinecatechins, derived from green tea extracts. The average time for clearance using this medication is 4 months. Another prescription topical medication that can be effective is imiquimod cream. It is an immune response modulator that increases gamma interferon production and has antiviral effects. Cryotherapy (freezing) is more effective than imiquimod or sinecatechins. Multiple treatments are required every 2-3 weeks. Cryotherapy is safe in pregnant women. Extremely large warts will require surgical removal.
Regular PAP smears can help detect cervical dysplasia due to HPV infection.
HPV Vaccine is highly effective against HPV types 6, 11, 16, 18. It has no therapeutic efficacy against an established HPV infection.
HPV 16 and 18 are responsible for 70% of genital warts.
Molluscum Contagiosum
Molluscum contagiosum is the most common infection in humans. It is caused by a poxvirus and is spread through direct skin to skin contact. It is a frequent skin infection in children. It can also spread through contact with contaminated objects. Molluscum contagiosum can also be sexually transmitted in adults.
The lesions are often mistaken for pimples. Molluscum contagiosum is typically asymptomatic; so individuals maybe unaware they are infected until large numbers of lesions appear on their skin. Molluscum may itch if they are located in areas on the body that are rubbed by clothing or in flexural areas such as armpits and groin. Squeezing, scratching, or rubbing molluscum bumps will spread the infection rapidly. Each little bump contains hundreds of poxvirus. Each microscopic viral particle can start a new infection.
Although molluscum may spontaneously resolve; a more typical scenario is the infection starts with a few bumps, which are ignored and the poxvirus multiplies merrily in the skin without interference into hundreds of lesions.

Molluscum contagiosum appear on the skin as pink or skin colored firm bumps. There is a little dimple in the center of the bump. Sometimes the dimple is filled with a whitish plug. Very large molluscum can hurt and become red and sore.

Dr. Wong recommends treating molluscum contagiosum as soon as the lesions appear. Skin that is well moisturized is less likely to be susceptible to molluscum infection because there will be fewer microscopic openings in the skin for the poxvirus to gain entry. Do Not share bath towels, underwear, or swimsuits.
Herpes Simplex Virus Infection (HSV)
There are actually 8 types of herpes viruses. For practical purposes, only types 1 and 2 will be discussed. Both HSV-1 & 2 infections can occur in the mouth, lips, and genital areas. Although HSV-1 has a predilection for the lips, face,
and mouth, HSV-1 can be spread to the genital areas by direct contact of infected skin. Similarly, although HSV-2 prefers infecting the anogenital region, HSV-2 can infect the oral region as well. The incidence of HSV-1 occurring on genital skin is increasing, presumably due to the increase in oralgenital sexual activity.
The earliest symptom of an HSV infection may be a sensitivity, burning, itching, or vague discomfort on the skin without any visible changes. Several days or weeks later, little blisters appear that are painful. The blisters are very
contagious and contain herpes virus. Direct skin to skin contact with the blisters can spread the virus to a new area. Fever, fatigue, painful lymph nodes, headache and flu-like symptoms are typical. Herpes lesions around the urethra
or anal area may be accompanied by difficulty urinating, burning with urination, anal itching, or painful defecation.
HSV infections are recurrent and the virus remains permanently harbored in the body. The vigilance of your immune system determines how well the virus is suppressed. Stress, lack of sleep, having a cold, etc. can cause HSV to
reactivate.

HSV can have several different appearances depending on the stage of the infection.

Initially, HSV appears as small shiny fluid filled blisters clustered together.

In the next stage, the lesions look like pustules. They appear as whitish or yellowish little bumps with redness of the surrounding skin.
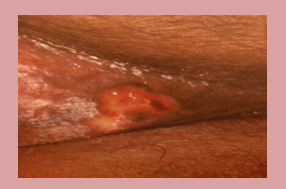
The blisters will eventually break and turn into open, raw, red, moist areas of skin. Sometimes this can look like "paper cuts" in the skin folds in the vulvar area or in the normal wrinkled skin on the shaft of the penis.

Herpes infection can occur even in the absence of any obvious herpes lesions on the skin. A large number of people are unaware they are infected with HSV. Asymptomatic shedding of the virus occurs even when one is taking
oral medication for the infection. HSV infection can be controlled with oral prescription medication such as valacyclovir, acyclovir, or famciclovir. The sooner medication is started, the faster symptoms and lesions will resolve.
Topical antiviral medication has minimal benefit over placebo. Condoms can provide some protection against infection. Individuals prone to frequent HSV outbreaks can benefit from chronic suppressive oral antiviral therapy.